Alleviation: An International Journal of Nutrition, Gender & Social Development, ISSN 2348-9340
Volume 3, Number 3 (2016) : 1-17
©Arya PG College, Panipat & Business Press India Publication, Delhi
www.aryapgcollege.com, www.apcjournals.com
Effectiveness of Continuous Glucose Monitoring in Diabetic Clinics
Dr. Nilima Varma & Prachi Chaturvedi
Professor, Research Scholar
Department of Foods and Nutrition, Govt SNGGPG College, Bhopal
(Madhya Pradesh), India
*Email: nvarma44@gmail.com
Introduction
Diabetes mellitus, commonly referred to as diabetes, is a group of metabolic diseases in which there are high blood sugar levels over a prolonged period. Symptoms of high blood sugar include frequent urination, increased hunger and increased thirst. If left untreated, diabetes can result in many complications, and acute complications include diabetic ketoacidosis, retinopathy, neuropathy, nephropathy, and cardiac problems etc. There are three major types of diabetes mellitus:
• Type 1 DM results due to the pancreas's failure to produce enough insulin.
• Type 2 DM begins with insulin resistance and in this, cells fail to respond to insulin properly. The primary cause is obesity and lack of enough exercise.
• Gestational Diabetes is the third main form which occurs when pregnant woman without a previous history of diabetes develops high blood-sugar levels.
Continuous Glucose Monitoring System
In the modern diabetes monitoring, Continuous Glucose Monitoring (CGM) could be considered as a third pillar, since it provides information on day-to-day change of blood glucose levels and helps achieving treatment targets without increasing the risk of hypoglycemia. A continuous glucose monitoring system is an approved device which records blood sugar levels throughout the day and night. It is inserted just under the skin of the abdomen and it works as a sensor. Every 10 seconds, the sensor measures the level of glucose in the tissue and sends the information to a cell phone-sized device called a "monitor" which can be attached to a belt or the waistline of the pants. An average glucose value is automatically recorded every five minutes for up to seven to fourteen days.
Hyperglycemia promotes the development of both long term complications and sub-optimal well-being in patients with diabetes. Glucometer readings obtained by finger pricks are at best, single “snapshot” providing reading at selected times over a 24 hours period. There may be patient bias to choose to test predominantly at times of low or high blood glucose levels and when preparing for review appointments.
Continuous Glucose Monitoring (CGM) enables tracking of blood glucose levels on continuous basis over 24 hour periods. This would enhance the diabetic patient’s awareness of excursion in glucose readings, particularly during nocturnal hours, when hypoglycemia may go unrecognized. It monitors glucose values in subcutaneous tissue fluid within a range of 40-400 mg/dl. Two weeks data of glucose can be stored in the monitor’s memory and then transferred to a personal computer for analysis. CGM lowers HbA1c without increase in the incidence or severe hypoglycemic episodes in patients with type1 diabetes who use the device frequently. Patients experience a positive quality of life.
This portable, pager sized device has a disposable glucose sensor attached which is inserted subcutaneously. The monitor acquires and stores electric signals from the glucose and converts these signals into clinical glucose values that are also stored. The monitor is required for seeing a blood glucose report. This device gives accurate result and easy to monitor blood glucose without any finger prick. Blood glucose sensor is a blood glucose monitoring device which gives ambulatory glucose profile. The objectives of present study are:
1) To identify the complications that occur in diabetic patients.
2) To know the awareness level for blood glucose sensor in diabetic patients.
3) To assess the biochemical parameters of the diabetic patient.
4) To counsel the diabetic patients for blood glucose monitoring device.
Methodology
In this study, 100 diabetic patients (Males & females) were selected from different diabetic clinics of Jabalpur city (Madhya Pradesh) in India. Data were collected by using general discussion and questionnaire which included closed ended questions for the convenience of respondents. Biochemical test techniques were used on the basis of category of sugar level (Low, moderate, high) in diabetic patients. Awareness for blood glucose sensor in diabetic patients was measured by general discussion and questionnaire method. Duration of diabetes, family history of diabetes, level of diabetes and awareness for glucose monitoring device and its use were also observed in diabetic patients. Counseling of diabetic patients was conducted to improve their health status and to promote the use of blood glucose sensor. Diabetic patients (Both males & females) were given educative booklets and pamphlets. They were also counseled through video demonstration for awareness towards sensor. Patients’ feedback was taken after one to three months. Feedback is taken back for knowing the level of awareness of patients.
Results and Discussion
Table 1 shows that the 26 per cent of the diabetic patients have normal level of blood glucose and 31 per cent of diabetic patients suffered from medium level of blood glucose and 53 per cent diabetic patients suffered from high level of blood glucose.
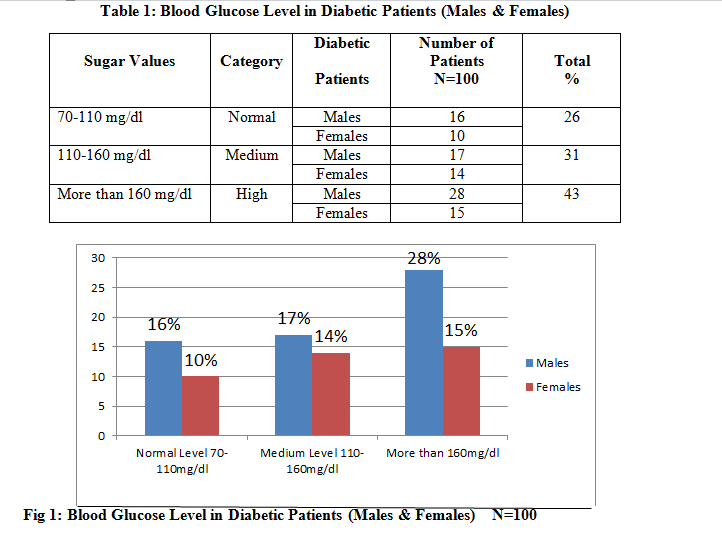
Table 2 shows that 41 per cent of diabetic patients suffered from retinopathy (Eyes problem), 19 per cent from neuropathy (Disfunction of nerves), 16 per cent from nephropathy (Kidney disorder), 14 per cent from cardiac problem and 10 per cent from other health problems.
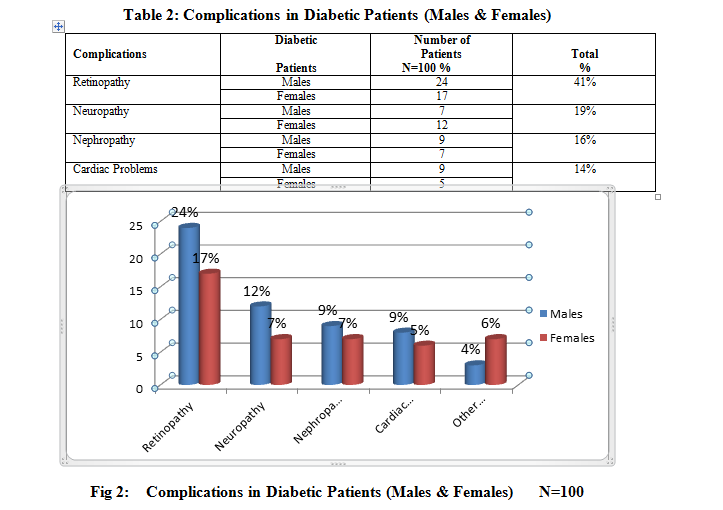
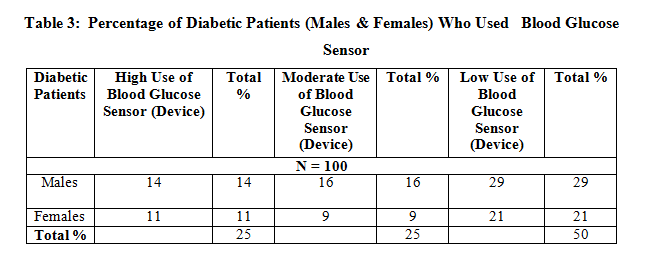
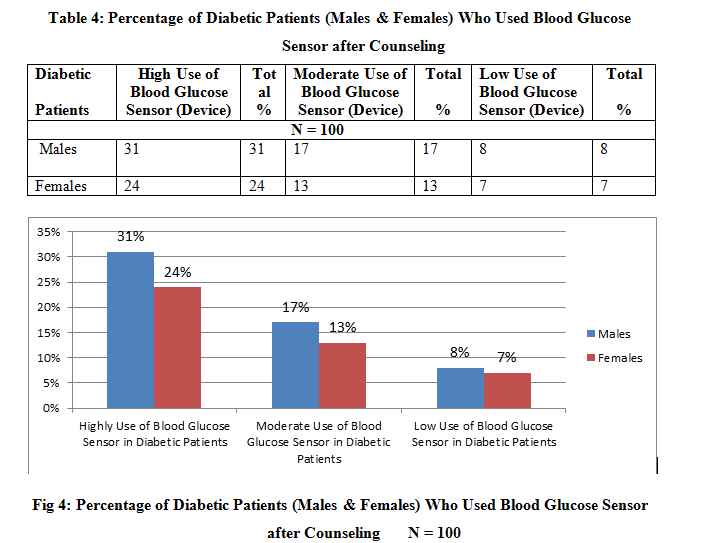
Table 3 shows that only 25 per cent of diabetic patients were aware of blood glucose sensor and they highly used this device for proper glucose monitoring and maintained blood glucose level. Apart from this, 25 per cent of diabetic patients made moderate use whereas 50 per cent made low use of this device. The results showed that the patients have a poor awareness regarding blood glucose sensor and proper monitoring of blood glucose.
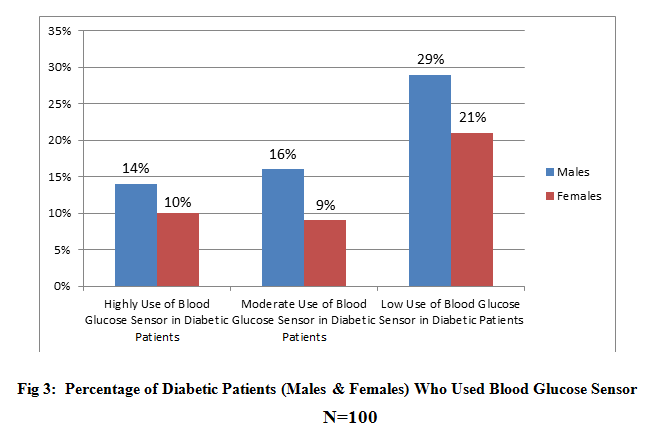
And after counseling, the use of blood glucose sensor was increased, it was found that 55 per cent of diabetic patients made high use of blood glucose sensor, followed by moderate use (30%) and low use (15%).
Conclusions
Current evidence shows that the real-time continuous glucose monitoring system has a beneficial effect on glycemic control in adult diabetic patients, without an increase in the incidence of hypoglycemia.
With the use of the sensor monitoring, several episodes of hyper and hypoglycemia could be identified.
The daily glucose summary graphs obtained with this sensor, help in counseling patients, dietary variations resulting in glycemic changes, can be visually explained. Blood glucose sensor is helpful in achieving better glycemic status in diabetic patients with the help of intermittent monitoring of sensor and maintaining blood glucose level.
In conclusion, real-time CGM systems can improve metabolic control, reduce hypoglycemic episodes and improve quality of life. Whether this holds true for longer time periods and in the majority of patients remains to be proven. In the long term, CGM might help to reduce chronic diabetes complications and perhaps also mortality, thereby reducing health care costs.
References
Diapedea (2014) Introduction to Diabetes Mellitus. Retrieved from www.diapedia.org/introduction-to-diabetes-mellitus.
International Diabetes Federation (2006) Diabetes Blue Circle Symbol. Retrieved from http://www.diabetesbluecircle.org.
Koul DM, Tarr JM, Ahmad SI, Kohner EM, and Chibber R (2012) Introduction to Diabetes Mellitus. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed.
Wikipedia -Diabetes Mellitus. Retrieved from https://en.wikipedia.org/ wiki/diabetes_mellitus.